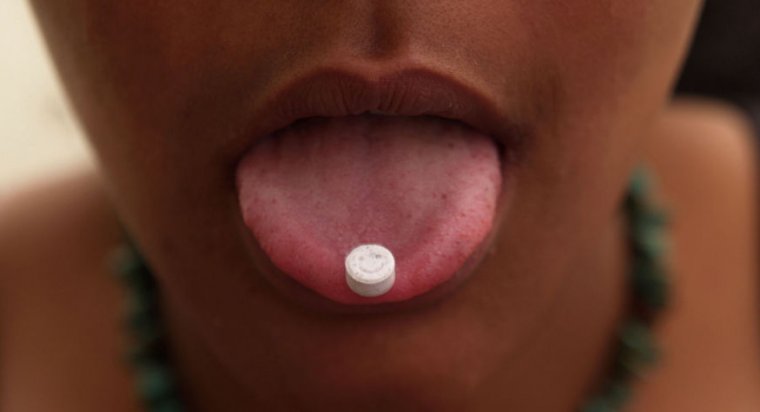
A corporation dedicated to studying the benefits of psychedelic drugs filed an application with the Food and Drug Administration this week for approval to use MDMA—aka ecstasy or molly—in combination with talk therapy to treat post-traumatic stress disorder.
If approved, it would be the first-of-its-kind combination treatment—a psychedelic-assisted therapy. An approval would also necessitate the Drug Enforcement Administration to reclassify MDMA, which is currently in the DEA’s most restricted category, plan I, which is defined as drugs “with no currently accepted medical use and a high potential for abuse.” The category also includes LSD, heroin, and marijuana.
The public benefit corporation (PBC) that filed the FDA application was created by MAPS, The Multidisciplinary Association for Psychedelic Studies, which has been supporting this type of work since 1986. The application is based on positive data from two randomized, double-blind, placebo-controlled Phase III studies, which were funded and organized by MAPS and MAPS PBC.
The first research, published in Nature Medicine in 2021, involved a total of 90 participants with moderate PTSD. It found that MDMA-assisted talk therapy (aka psychotherapy) significantly improved Clinician-Administered PTSD Scale for DSM-5 (CAPS-5) scores compared with participants who were given talk therapy with a placebo. In the second research, published in September in Nature Medicine, the finding held up among 104 participants with moderate or severe PTSD (73 percent had severe PTSD).
In both trials, participants took 80 to 180 mg doses of MDMA or a placebo at the start of three eight-hour sessions, which were spaced around a month apart. Between those experimental treatment sessions, participants also had three 90-minute sessions for participants to process the experimental experience.
MDMA—3,4-methylenedioxymethamphetamine—affects neurotransmitters in the brain, increasing the activity of serotonin, dopamine, and norepinephrine, to be specific. This leads people who take the drug to experience euphoria, hallucinations, sharpened sensory perception, and sociability, but it can also bring about confusion, depression, and paranoia. Its use in psychotherapy has been explored for decades.
In a statement this week, MAPS PBC CEO Amy Emerson celebrated the FDA submission. “The filing of our [new drug application] is the culmination of more than 30 years of clinical research, advocacy, collaboration, and dedication to bring a potential new option to adults living with PTSD, a patient group that has experienced little innovation in decades,” she said.
MAPS founder and President Rick Doblin also celebrated the submission this week, saying in a statement: “When I started MAPS in 1986, the FDA was still blocking all research with psychedelics. … By breaking that barrier, we have opened doors for others to conduct their own promising research into psychedelic-assisted therapies with psilocybin, ayahuasca, ketamine, and more. The novel approaches undertaken in psychedelic-assisted therapy research have led to fundamental shifts in our understanding of how these devastating mental health conditions can be treated.”
So far, the MDMA-assisted therapy has drawn criticism for its expected inaccessibility. The treatment outlined in the two MDMA trials involves lengthy—and likely pricey—therapy sessions with highly trained therapists. The Washington Post published an estimated price of between $13,000 to $15,000 per treatment round, and it’s unclear for now whether it would be covered by health insurance if approved by the FDA. “Most people in the world won’t be able to afford these clinics,” Allen Frances, a Duke University professor emeritus of psychiatry, told the Post.
Now that the NDA is submitted, the FDA has 60 days to set up whether it will be accepted for review and whether it will be a priority or standard review (six months or ten months, respectively), MAPS PBS noted. MAPS is seeking a priority review. In 2017, the FDA granted MDMA “Breakthrough Therapy,” designed to help expedite the development and review of drugs for serious conditions when evidence indicates they may substantially better upon current therapies.
The only psychedelic with FDA approval to date is esketamine, a variation of ketamine, which was approved in 2019 to treat treatment-resistant depression.

