The pain has been described as agonizing, searing and excruciating.
Having a highly effective contraceptive called an intrauterine device (IUD) inserted can cause significant discomfort for some people, and a growing chorus of health-care professionals and patients has been calling for better pain management during the procedure.
Now, a Planned Parenthood location in the U.S. has made headlines for announcing it will start offering routine sedation to patients during IUD insertions and removals, explaining that accessing reproductive health care shouldn’t invoke fear, and that the procedure “shouldn’t feel traumatizing.”
But as some people applaud the move, the president of the Society of Obstetricians and Gynaecologists of Canada (SOGC) says routine sedation has the potential to limit access to a highly effective form of contraception.
While sedation can be offered to some patients here who can’t tolerate the insertion in an office setting, it requires more monitoring, emergency services and an outpatient surgical suite or an operating room, said Dr. Amanda Black.
That can be limiting, she said.
White Coat Black Art26:30The trouble with IUDs (Part 1)
IUDs are an effective and popular form of birth control in Canada. But many women experience intense pain from the insertion that they weren’t warned about. In this episode, women across the country share stories of unexpected pain, complications and emotional distress. In Part 2, what some gynecologists are doing to make the experience of getting IUDs more comfortable.
“We don’t do it routinely,” Black told CBC News.
She said sedation is not something most providers can do in an office setting, and not all practitioners have easy access to an operating room.
“We can’t minimize the fact that people have had unpleasant experiences with IUD insertions. What we need to do is figure out how to improve that experience for them moving forward.”
‘Way too common’ for patients to not get any pain management
About 159 million people worldwide use IUDs, according to 2019 data compiled by the United Nations. It was the third most common form of contraception globally, after female sterilization and male condoms, and just above the pill.
It’s also one of the most effective forms of birth control, and a “recommended first-line contraceptive method,” according to the SOGC.
The SOGC describes IUD insertion as a rapid outpatient procedure that can be completed in five to 15 minutes.

During the procedure, a small, T-shaped device is inserted through the cervix into the uterus. In its insertion guide, the SOGC mentions the possibility of “brief moments of sharp pain,” especially when the device passes through the cervix.
Some small studies have found most people describe moderate to severe pain during insertion. Social media platforms like TikTok are full of people describing their negative experiences.
One study of the top 100 videos tagged #IUD on TikTok found that all of the videos conveying patient experiences had a negative or ambiguous tone, and almost 97 per cent highlighted pain and other side effects.
It’s “way too common” for patients not to get any pain management while undergoing the procedure, Dr. Joss Reimer, the Winnipeg Regional Health Authority’s chief medical officer, said in a 2023 interview with CBC Manitoba‘s Information Radio.
“It’s a long-standing practice where we just don’t value the pain of women the same way we do men, and expect them to go through painful procedures that we wouldn’t expect in other circumstances.”
Information Radio – MB7:33IUD pain and doctors
It can be one of the most painful experiences for a women…but it’s not common for the pain to be managed. Dr. Joss Reimer shares with guest host Faith Fundal why despite its benefits IUDs are so controversial
In a statement on April 2, Dr. Colleen McNicholas, the chief medical officer at Planned Parenthood of the St. Louis Region and Southwest Missouri, said the organization has been listening to people calling for better pain management solutions and will now offer sedation for “patients who prefer it.”
“We’re offering sedation to give patients a greater sense of power and control over their bodies and their care,” McNicholas said.
Several other Planned Parenthood locations in states in the U.S., such as Massachusetts and Arizona, appear to offer oral and intravenous sedation, as well.
They note that sedation carries increased risk, and patients will not be able to drive themselves home afterward.
Pain management options
Every patient is different, and it’s important not to dismiss the pain and discomfort someone may experience, said Black, with the SOGC.
“We can definitely do better than we have in the past, and we are making changes to how we do our IUD insertions because of that,” she told CBC News.
Those changes include taking a more individual approach, she said, and telling patients ahead of time that they may experience discomfort and cramping — some much more than others. Doctors should also make sure patients understand that they’re in control, and can stop the procedure or take a break at any time.
“In the past, we were somewhat reluctant to use any type of pain medication or anesthetic to try to help with the procedure, because we thought it would actually hurt more to do that, but I don’t think that’s necessarily the case for all patients,” Black said.
But there are options.
Patients can take anti-inflammatory medications ahead of time or immediately after the insertion, she said, and doctors can be ready to inject a local anesthetic or use an anesthetic spray.
And just recently, there’s the option to use an inhaled pain medication that the patient controls themselves during the procedure, Black said.
“At the end of the day, the majority of patients do well.”
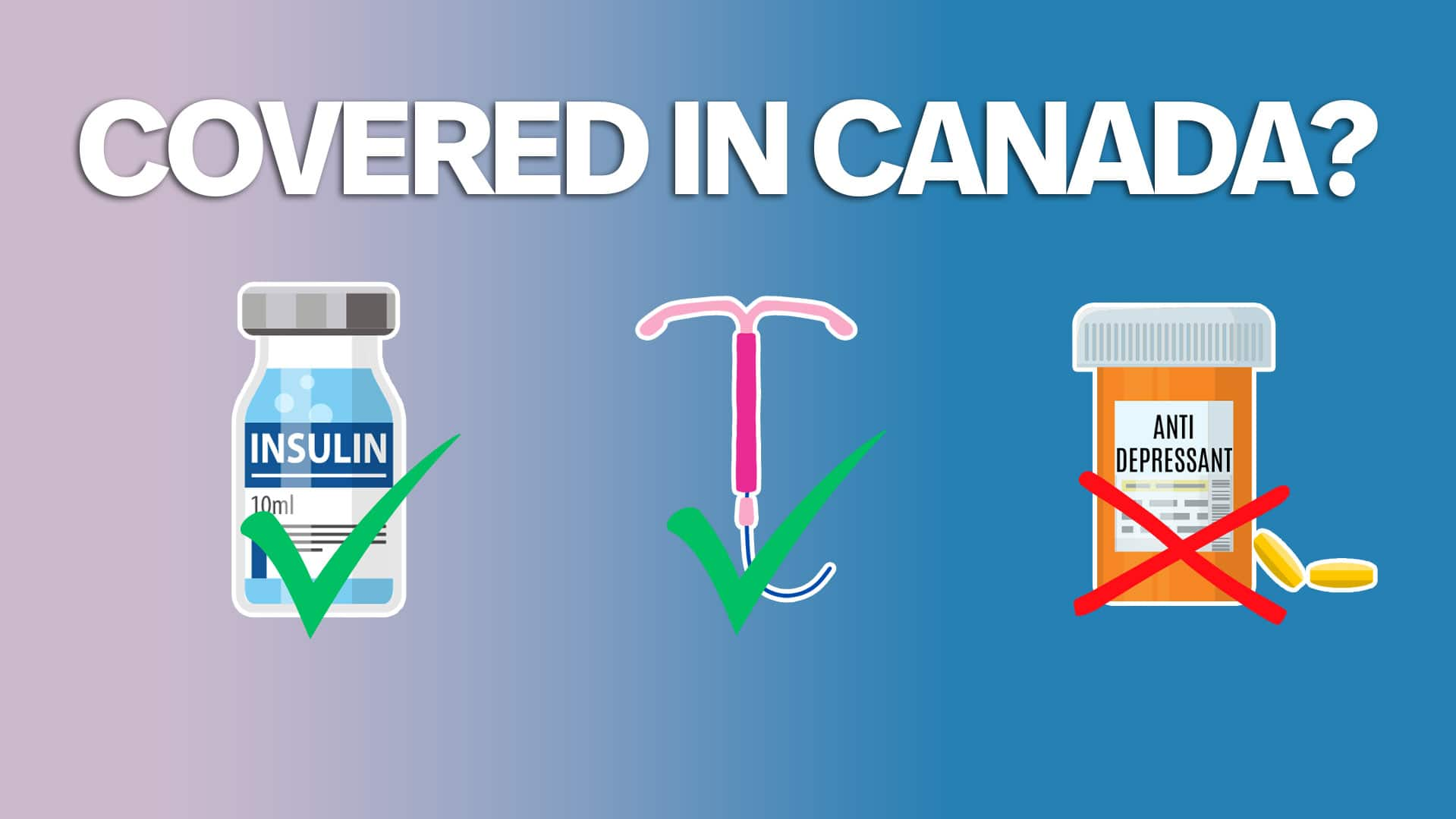
The federal Liberal government and the NDP have agreed on a framework for new pharmacare legislation, paving the way to making some prescription drugs free in Canada. Andrew Chang examines why the first phase of the proposed plan will cover some contraception and diabetes treatments, and what questions still remain.