Diagnosis and treatment delays are hurting and even killing cancer patients.
Article content
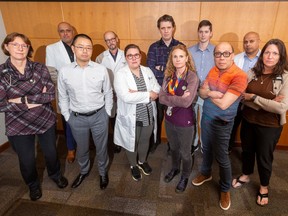
While cancer care has improved for Alberta patients in terms of treatment, leading to better outcomes, there aren’t enough doctors, leading to delays in diagnosis and treatment, a leading oncologist says.
Dr. John Walker, the division director for medical oncology at the Cross Cancer Institute, said revolution in cancer care in the last decade means a buffet of treatment options: immune therapies, targeted therapies, chemo, surgery and radiation spell healing success for more patients than ever.
Advertisement 2
Article content
Article content
“Patient survival has dramatically increased across a whole range of cancers,” Walker said.
“The majority of patients will receive a non-chemotherapy treatment from a medical oncologist,” he added.
Heartbreaking numbers
More people are moving to Alberta, Albertans are living longer, and there are more oncology treatments because of technology. Those oncology treatments are becoming more successful. So cancer rates are getting higher.
That makes more cancer patients — and more cancer survivors, who may need more cancer care late — but we don’t have more oncologist.
Those we have are feeling “disheartened,” said Dr. Paul Parks, an emergency physician who heads the Alberta Medical Association.
“There’s moral injury and distress when they see patients that could have been cured, had they got to see them in time — and now they can only offer them palliation or treatment that will just prolong their life for a bit of time when they could have been cured,” Parks said
“That takes its toll, for sure.”
Alberta’s target is for patients to see an oncologist within four weeks from the diagnosis of cancer.
Article content
Advertisement 3
Article content
It can take up to eight weeks to be seen by a medical oncologist, up to 13 weeks to see a radiation oncologist.
Consider a young woman with breast cancer. A small lump that gets diagnosed, there’s a lumpectomy and the bit of cancer taken out by surgery needs radiation to avoid recurrence.
But because of delays for the radiation oncologist, that cancer is back and another surgery’s required before she even gets to see the specialist.
Then there’s the well-known shortage of family practitioners who might flag a symptom, a mole, a lump.
“If you don’t have a family specialists, these cancers get delayed further into their course,” Parks said.
Now, emergency doctors are too often the first to see undiagnosed advanced cancers — not the best place to get a diagnosis of cancer, Parks said.
Despite efforts to streamline treatment, there’s delays getting to the oncologist.
The kicker? If cancer isn’t addressed early, patients need more surgeries, more time in the hospital. That impacts Alberta’s bed shortage.
Lagging behind: Recruit, retain
Most of the cancer care in Alberta is centralized within the two main cities, with 27 full-time oncologists at the Cross in Edmonton and about the same in Calgary.
Advertisement 4
Article content
The Cross Cancer Institute had 4,837 new patients in consultation in 2023.
Five years ago, there were just under 4,000 patients going into the care system.
That’s a 20 per cent hike.
Plus there are indispensable regional cancer centres in Grande Prairie, Medicine Hat, Red Deer, and Lethbridge, each with an oncologist or two — also woefully understaffed, Walker said.
Canada’s premier cancer centre will open in Calgary within months.
“But we don’t have enough bodies. There just aren’t enough oncologists or care providers to make sure that our patients are getting into the carestream in timely fashion, and to make sure they’re being appropriately and comprehensively cared for while they’re receiving these really exciting therapies,” Walker said.
“Over the past 10 years, we haven’t created new spots for oncologists. The workforce has been largely static,” he said.
Funding is different for oncologists, who work under Cancer Care Alberta, a branch of Alberta Health Services.
For an oncologist to practise in Alberta, they have to be a contractor to a specific position within Cancer Care Alberta.
Advertisement 5
Article content
Oncologists are typically salaried; the traditional fee-for-service model isn’t amenable to complex cancer care.
“We haven’t seen the number of oncologist positions increase to keep pace with even population growth. Of much more importance is this transformation of the care that we’re delivering and providing that just needs far, far more resources,” Walker said.
Alberta Health Services confirmed the demand for cancer care has steadily increased year after year.
“We are working to address this, including exploring options such as extending clinical hours to reduce wait times wherever possible,” said spokesman Kerry Williamson.
“AHS continues to aggressively recruit for all frontline staff, including oncologists. This year, 17.2 FTE Cancer Care Alberta physicians have been recruited with various start dates in ’24/’25,” he said.
“Ensuring Albertans have timely access to cancer care is a priority for AHS and we are doing everything we can to recruit for positions throughout cancer care, including medical oncology, medical physics and radiation therapy.”
Advertisement 6
Article content
The new Arthur JE Child Comprehensive Cancer Centre in Calgary is expected to attract international experts through active recruitment using multiple strategies, including international recruitment campaigns in the U.S. and U.K., and working with several post-secondary institutions to provide practicum supports, he said.
Where the action is
B.C. is building several new cancer centres, and they’ve proactively recruited hired 350 cancer care professionals in the last year alone, including about 60 oncologists.
Ontario picked up the pace a few years ago.
“I think Alberta used to do a very good job of making physician positions attractive — and part of that was remuneration. We’ve definitely fallen behind our neighbouring provinces over the last decade,” Walker said, noting an even larger stumbling block.
“When you fall below a certain critical threshold of oncologists and allied care providers, now you become a jurisdiction that becomes unattractive just because you’re trying to draw new bodies into an environment that’s already under stress and duress. There’s an urgency to start creating these new positions for oncologists.”
Albertan born and bred, Walker’s been at the Cross Cancer Institute for 15 years, with no plans to uproot.
“But if you’re a new graduate, and you have a choice of where to live and practise … we need to be competitive with jurisdictions like British Columbia, to make sure that these new individuals will choose Calgary or Edmonton or Grande Prairie or Red Deer. And we’re not at the moment,” he said.
“That needs to change.”
Article content



