The Dose25:46How should I treat migraine attacks?
The stereotypical image of a migraine sufferer is someone lying in a dark, quiet room for hours with an ice pack on their head.
And while that is still true in some cases, new effective medications specifically designed for migraine have changed the outlook for many patients of this often misunderstood neurological disorder, experts say.
“The problem with migraine is that a lot of people endure a lot and they’re not treated properly,” said Dr. Elizabeth Leroux, a neurologist in Montreal specializing in headaches and migraine.
“I see a lot of patients who know more than their doctors sometimes,” Leroux told Dr. Brian Goldman, host of CBC’s The Dose.
What is a migraine?
Unlike a regular headache that only involves head pain, a migraine is a neurological event that usually comes with other symptoms — nausea, vomiting, sensitivity to light and noise, neck pain and a visual aura are all possible.
Frequency can vary, and chronic migraine is defined as having a headache at least 15 days per month, with at least half of them having migraine symptoms.
Compared to a tension headache, a migraine is often disabling, said Dr. Lara Cooke, neurology professor at the University of Calgary.
“If you wish you could turn down the volume on the world, or you could turn down the brightness of the sun … likely it’s a migraine,” said Cooke, who has a specialty in headache medicine.
What causes migraine?
Though the exact science behind migraine isn’t fully understood, researchers now understand more about the nature of the pain, according to Leroux.
Migraine pain comes from an interaction between the trigeminal nerves and certain systems in the brain, said Cooke.
The two trigeminal nerves run down each side of the face and send touch and pain sensations from the face to the brain.
When something triggers a migraine, those nerves get fired up and release calcitonin gene-related peptide (CGRP), a brain chemical that interacts with blood vessels in the head, causing throbbing pain.
Who gets migraines?
Migraines can start in childhood and affect all genders. Research shows that after puberty, more women than men experience migraine.
Some migraines are tied to the menstrual cycle and often improve post-menopause.
“It’s very clear that ups and downs with estrogen play a very important role in migraines in women,” said Cooke.
Some hormones, including progesterone and oxytocin, make the female brain more prone to chronic pain diseases in general, including migraine, said Leroux.
Migraine triggers
Experts say there are a few common migraine triggers, such as alcohol, lack of sleep, and weather changes. They differ for everyone, so it’s worth figuring out your individual triggers.
A common theory around migraine is that everyone has a threshold for their triggers, and if several triggers coincide and the threshold is surpassed, a migraine will follow.
“You had a bad sleep, you’re stressed, and then you had a glass of red wine … the sort of perfect storm,” said Cooke.

Managing your triggers can help with migraine, but it can only go so far, said Leroux.
“Sometimes your threshold is so low that just living and going to work and doing things with your family is unbearable,” she said.
“And that’s where I think medical care comes in.”
New medications for migraine
There are two general categories of medication to treat migraine: those that treat a migraine attack, and those that can prevent attacks.
Medications used to treat acute migraine attacks usually include a category of prescription drugs called triptans. Over-the-counter medications, including anti-inflammatories such as ibuprofen and naproxen, can help treat some of the milder symptoms.
Doctors have also been prescribing various medications to try and prevent migraine attacks, or at least reduce their frequency and/or intensity, for many years, all originally designed to treat other conditions such as epilepsy, depression or high blood pressure.
But for some with frequent migraine, a new category of preventive medication called CGRP blockers, or anti-CGRP monoclonal antibodies — designed specifically to treat migraine — has made a huge difference, said Leroux.
“[Patients] come to me after decades of migraine — their life has changed … they don’t fear the next attack,” she said.

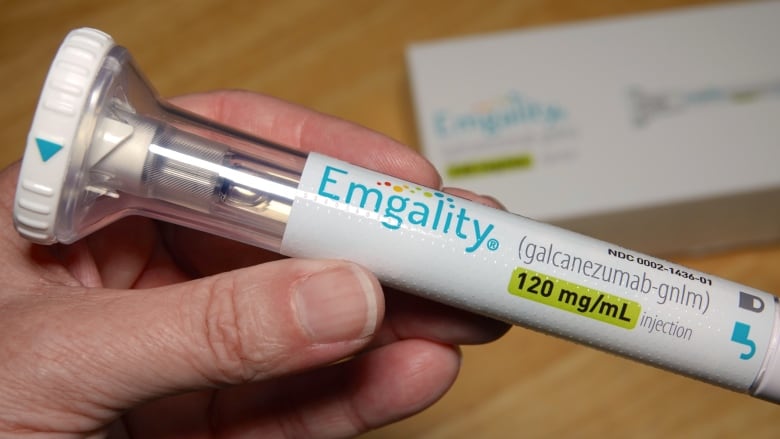
These medications — which came onto the market in 2018 — block CGRP (calcitonin gene-related peptide), a brain protein that dilates blood vessels and causes the pain of a migraine attack, and can reduce the intensity and frequency of migraine attacks over time.
There are four such medications approved in Canada: erenumab, fremanezumab, galcanezumab and eptinezumab — sold under the brand names Aimovig, Ajovy, Emgality and Vyepti. Patients self-inject them, usually once a month.
Another class of CGRP antagonists, known as gepants, come in pill form and can be used to treat acute migraine attacks or preventatively. Three are approved in Canada: ubrogepant, rimegepant and atogepant — sold under the brand names Ubrelvy, Nurtec and Qulipta.
CGRP medications are expensive, costing more than $600 per injection and around $20 per tablet, and not all provincial drug plans fully cover them. Coverage by private insurance plans varies.
Relief from new drug
Christina Sall has been taking the anti-CGRP antibody Aimovig (erenumab) since 2019 and said it has been “the best experience.”
Sall, a registered nurse from Surrey, B.C., started getting migraines when she was five years old.
As a teen, the attacks intensified. They became so bad in her early 20s that she had more than 15 days a month with a migraine.
Sall tried preventive medications, but they didn’t work and gave her terrible side effects, even landing her in the emergency room.
“Being dismissed at the ER that these aren’t even real symptoms and that I’m just having anxiety is really frustrating,” Sall said.
“It was a really, really dark time in my life.”
Sall’s migraines were so bad that she was forced to drop out of school during her nursing degree, but after taking anti-CGRP antibodies was able to return.
CGRP blockers aren’t effective for everyone, cautioned Leroux, but she said that if they work for you, they can vastly improve your quality of life.
Botox injections were approved as a preventive for chronic migraine in Canada in 2011 and have been shown to be effective for some patients, say experts.
The toxin in Botox gets taken up in the nerve endings and prevents the nerve from releasing neurochemicals that it’s believed cause migraine pain, said Cooke.
In order to be approved for Botox, patients often need to confirm that they tried other preventive medications that didn’t work.
Sall is grateful for the advances in migraine treatment in the past few years, but cautioned it can be challenging for each individual to find medication that works.
“It does take time to make sure that you’re on the right track,” she said.
“Changes to your lifestyle can help to an extent, but it isn’t going to miraculously get rid of migraine. It is a neurological disorder.”



