White Coat Black Art26:30Preventing the next Belleville
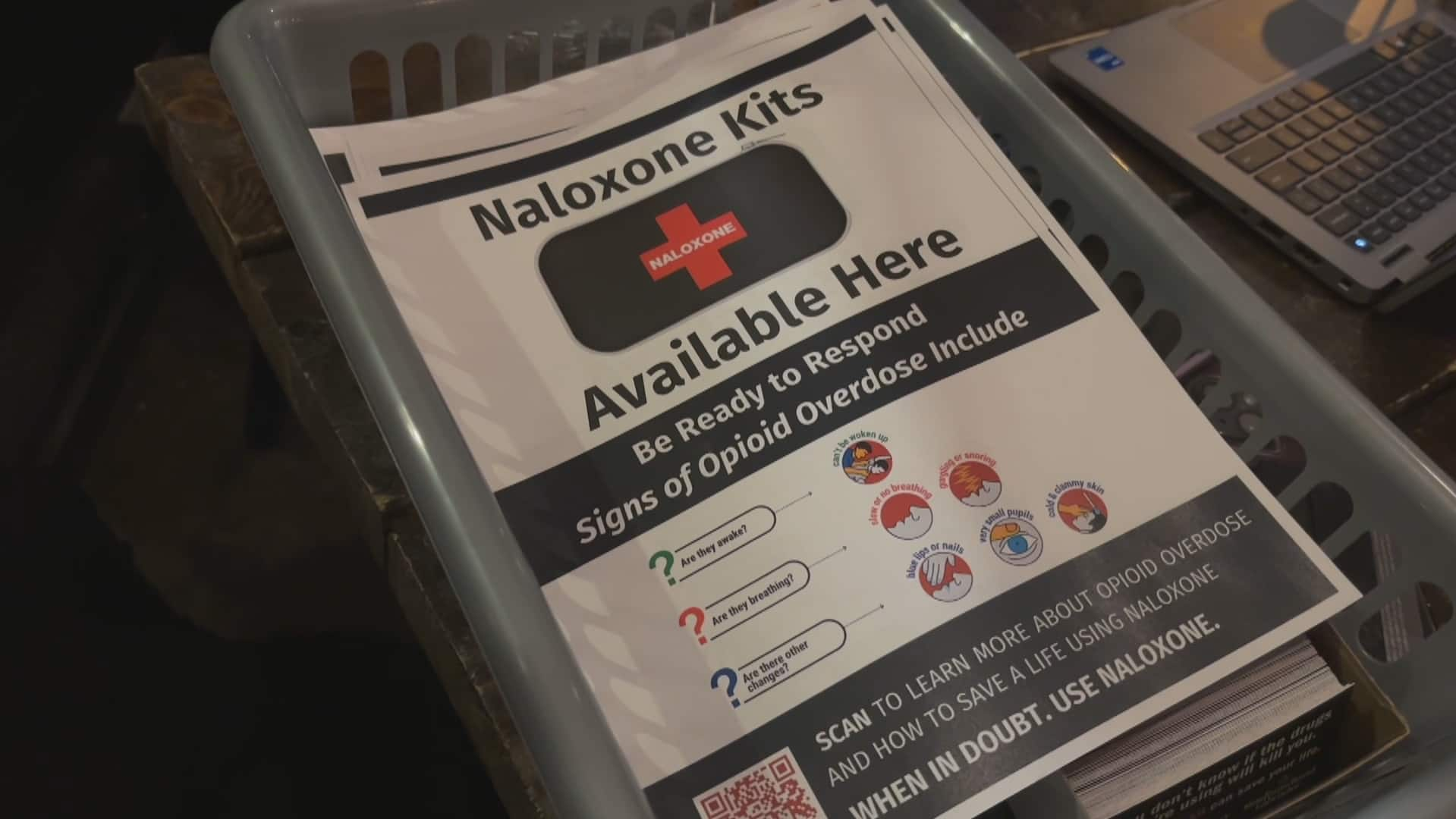
At The Mill on Main restaurant in Huntsville, Ont., manager Michelle Francis is placing a naloxone kit near the wood-burning pizza oven behind the bar, within easy reach for staff — just in case.
“It has two nasal sprays in there,” she told White Coat, Black Art‘s Dr. Brian Goldman. “I do remember in the training, sometimes you’ll have to use two if the first one doesn’t work.”
“I hope we don’t ever have to use it.”
Francis and her co-worker recently finished training that teaches them how to use naloxone — a drug that can help reverse an opioid overdose or poisoning — for the workplace.
Since June 1, 2023, Ontario workplaces considered at risk of worker opioid overdoses must carry at least one naloxone kit and undergo mandatory training. If they don’t comply, they could be fined.
However, some businesses that aren’t required to take the measures are still choosing to do so, like The Mill on Main. It’s not considered high risk, but after finding drug paraphernalia in the customer washroom one day, Francis decided to be proactive.
It’s one tool among many, including learning CPR and rescue breathing, needed to fight the ongoing opioid crisis, which can hit smaller communities harder than large cities.
People living in small towns hope that spreading awareness can also help dispel the stigma of drug use and avoid a worst-case scenario, like in Belleville, Ont., where 23 people overdosed in just 48 hours.
Mandatory training and kits for at-risk workplaces
Under amendments to Ontario’s Occupational Health and Safety Act, for a workplace to be required to have naloxone kits, these three scenarios must apply:
- There is a risk of a worker opioid overdose.
- There is a risk someone overdoses while in a workplace where they perform work for the employer.
- The risk is posed by someone who performs work for the employer.
The legislation only covers employees at their workplaces, and not members of the public, like customers or patients.
The kits and training on their use, provided by third-party organizations like St. John’s Ambulance, were free until March 31; Ontario provided kits to two employees per at-risk workplace. The government’s funding for it has since ended, and workplaces now have to pay up — including those at-risk businesses for which it’s mandatory.
As of February, more than 5,000 workplaces have participated in the Ontario government’s Workplace Naloxone Program, according to a labour ministry spokesperson. Over 4,300 free nasal spray naloxone kits were distributed to businesses, and more than 4,800 workers were trained to administer the medication.
Several WNP training providers continue to offer training to employers who request it, at a cost of $30 to $40 per person.
A representative for St. John’s said its online training teaches attendees how to recognize the signs of an opioid poisoning, administer oxygen and identify potential complications of administering naloxone.
It also includes brief sections on CPR and rescue breathing, as street opioids these days might also be adulterated, making naloxone less helpful.
Greatest demand from workplaces not at risk
The greatest demand for the WNP training actually came from workplaces that weren’t mandated to do it, according to Matthew Budau, an occupational health and safety advisor for Health & Safety Professionals Inc., an Ontario-based training and consulting firm.
“We heard a lot of people saying that they wanted to be ready if something happened in their workplace,” said Budau.
For Nici, a server at The Mill on Main, undergoing training came with a personal reason: Her sister Sadie died last year from opioid poisoning, at the age of 38.

CBC News has agreed to not disclose the sisters’ full names, as Sadie’s husband hasn’t yet told their two young children the details of their mother’s death.
“I wanted to better equip myself, because I know how quickly things can take a turn for the worse,” Nici said.
Stuart McKinnon, deputy chief of Muskoka Paramedic Services, says training laypeople in these skills is critical, since his team of responders alone isn’t enough.
Last year, he said, his team administered naloxone seven times, but responded to about 50 cases of suspected opioid-related poisonings.
Of those cases, 17 received naloxone from bystanders.

It’s also important because addiction doesn’t always look like one thing.
“Society visualizes drug addicts as what you see on TV, what you see on streets,” said Francis. “But it’s not [always]. It’s your soccer mom. It’s your dad. It’s your cook in the kitchen.”
According to a July 2022 report from Public Health Ontario, the construction industry is disproportionately affected by the opioid crisis. Francis says restaurants aren’t immune to the risks, either — even an upscale cottage-country location like The Mill on Main.
Fighting stigma
McKinnon says the WNP training is key to fighting the stigma around drug use to ensure people feel comfortable to help those in need, rather than hesitating or walking away — those seconds or minutes before emergency responders arrive can mean the difference between life and death.
Canada’s Good Samaritan Drug Overdose Act is designed to encourage bystanders not to flee the scene. It provides legal protection to bystanders of someone who is overdosing, who are also using drugs or have them in their possession. It also protects people from liability for trying to help at the scene of an overdose.
The Newfoundland Embassy in downtown St. John’s recently hosted dozens of people who practised administering naloxone — to inanimate objects — under the watchful eye of two provincial harm reduction workers. The CBC’s Jessica Singer dropped by and learned even more bar and restaurant staff are being trained in what could be a life-saving skill.
“We need to get away from the liability fear … [and] get more into the idea of, ‘I’m here to help this person and I shouldn’t worry about anything else; as long as I’m doing with what’s within my scope and what’s expected of me to help this individual, I’ll be fine,'” he said.
For Nici, even taking the first steps to learn how to deal with an opioid emergency can help avoid tragedies like her sister’s death.
“These people don’t want to die. She didn’t want to die. She wanted to get through it and get away from it. It’s just such a powerful, scary thing when you lose control.”