A University of Alberta professor is testing a new portable ultrasound machine that he says could drastically reduce emergency room wait times.
Abhilash Hareendranathan, assistant professor in the Department of Radiology and Diagnostic Imaging, said upper limb injuries are responsible for at least one out of every five emergency room visits in the country. His new machine scans for wrist and elbow fractures or tears in the rotator cuff.
He chatted with CBC Edmonton’s Radio Active about his machine.
The conversation has been edited for length and clarity.
Radio Active: So what is this new ultrasound device that you have here in front of you?
Hareendranathan: We basically have an ultrasound probe that can literally attach to a smart phone or a tablet. Now, you can see how this is going to be quite transformative because what that means is instead of getting the patients to the technology, you can take the technology to the patients. I just walked in with this device right here, and I could be performing a scan right on the spot. The advantage we see with this is we can completely transform the way fractures or injuries of the upper limb are examined in the emergency departments across Canada.
What we propose is instead of [waiting for an x-ray], we give one of these to the triage nurse. The nurse is able to perform a quick scan of the wrist or elbow or shoulder which are the most common places where you might have an injury.
RA: You mentioned some of the injuries like wrist, elbow, shoulder. What other uses could it to help with?
Hareendranathan: This is a general ultrasound probe, so it can be used for any kind of ultrasound examination. For example, another use case we see for this — as a separate project — is to perform a simpler examination of the heart. So right now the wait list for getting an echocardiograph is pretty long because it’s a pretty lengthy examination.
Now with this technology, we can make the whole thing simpler and it can be ideally, if it could be performed by a primary care physician in a primary care centre, that completely changes the way in which care is administered. And especially you can see how that is quite transformative in rural and remote communities, where there’s not access to an elaborate hospital infrastructure.
LISTEN | The machine would require minimal training:
Radio Active7:31AI-powered ultrasound device could shorten emergency waits
We meet Abhilash Hareendranathan, the local researcher behind a portable ultrasound device that could change how people with arm, wrist or shoulder injuries are triaged by emergency department staff.
RA: Compared to a regular ultrasound piece of machinery, is this much smaller?
Hareendranathan: Yes. When we think of an ultrasound, most of us have the picture of the fridge-sized ultrasound machine that’s connected, which is generally the one that’s used in hospitals. This is miniaturization, and where we come into play is developing the apps that have artificial intelligence in them, because one of the challenges that we still face with ultrasound is with this transformative technology, you would expect this to be used all over the place.
But one of the reasons it’s not is because people are hesitant to perform these examinations without assistance or some kind of feedback on the quality of the images that they acquire.
What we try to do is to use artificial intelligence and automatically assess the quality of these images and try to provide suggestive findings on them.
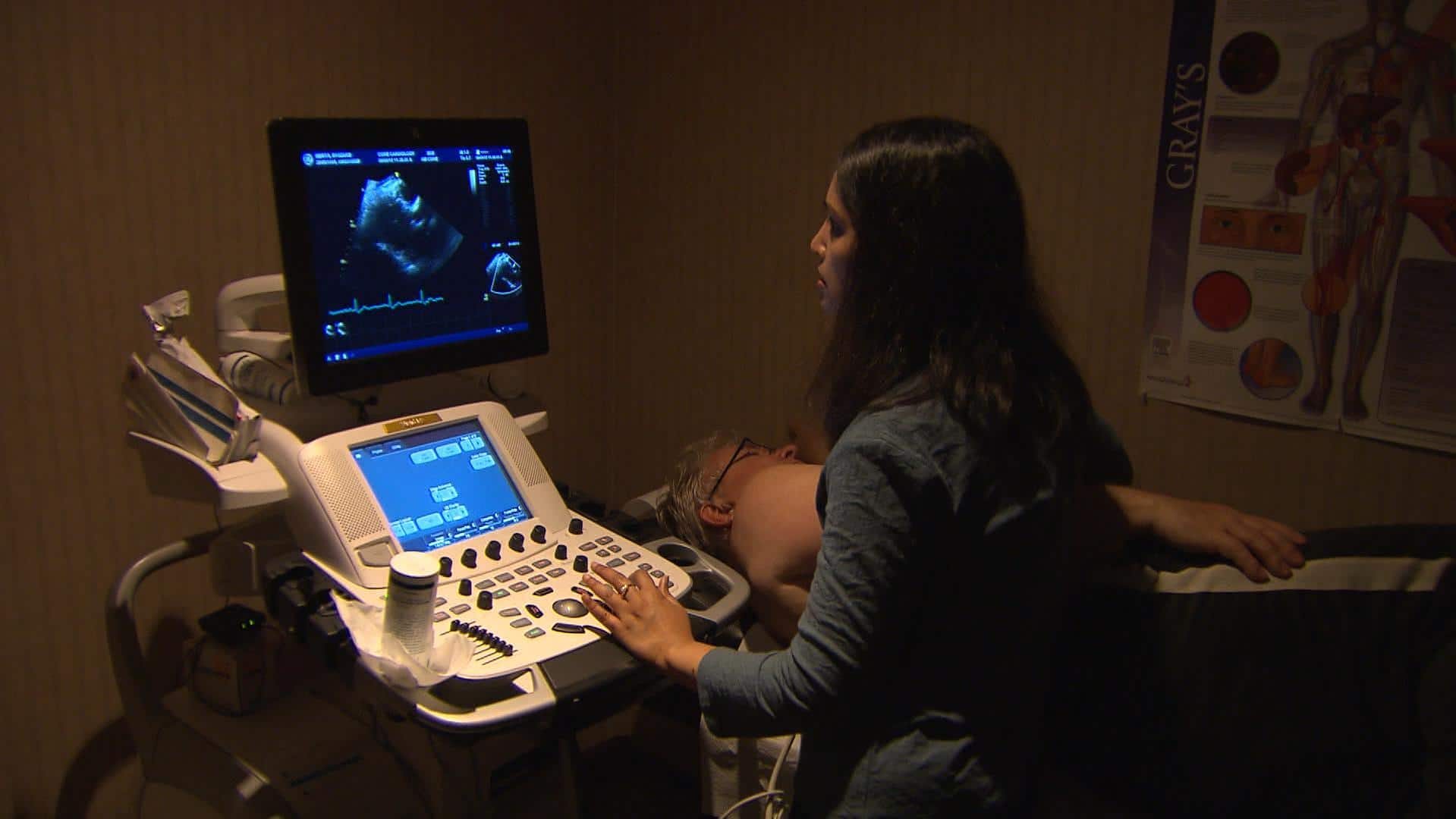
WATCH | An Edmonton researcher working on a pocket-sized ultrasound device:
An Edmonton researcher is working on a pocket-sized ultrasound device that could help get people out of emergency rooms quicker. Abhilash Hareendranathan is an assistant professor with the University of Alberta’s faculty of medicine and dentistry, and he joined CBC’s Min Dhariwal to tell him all about it.
RA: What kind of trials are you going to be doing with this device in the near future?
Hareendranathan: The plan is to perform a validation in the emergency department in the Stollery Children’s Hospital.
We see this as a pediatric use case because there, we are cutting down the risk of radiation from X-rays. The plan is when we have this up and running in the next two years, we perform this from the emergency department triage station in the Stollery.
RA: From what I understand, you’ve already been running some trials for this device. What’s been the reaction from health-care professionals who’ve been using this?
Hareendranathan: It’s hugely positive, I would say, because it’s a win-win. It’s a win for the patients because they do not have to endure the long wait times and it’s a win for the nurses because right now, I would say the triage station is a little bit underused because there’s not much that you can do without a diagnostic device. But now this is empowering the existing user. The key idea we have is to get this to users who are already part of the health-care system and to enable them to perform these exams with minimal training.